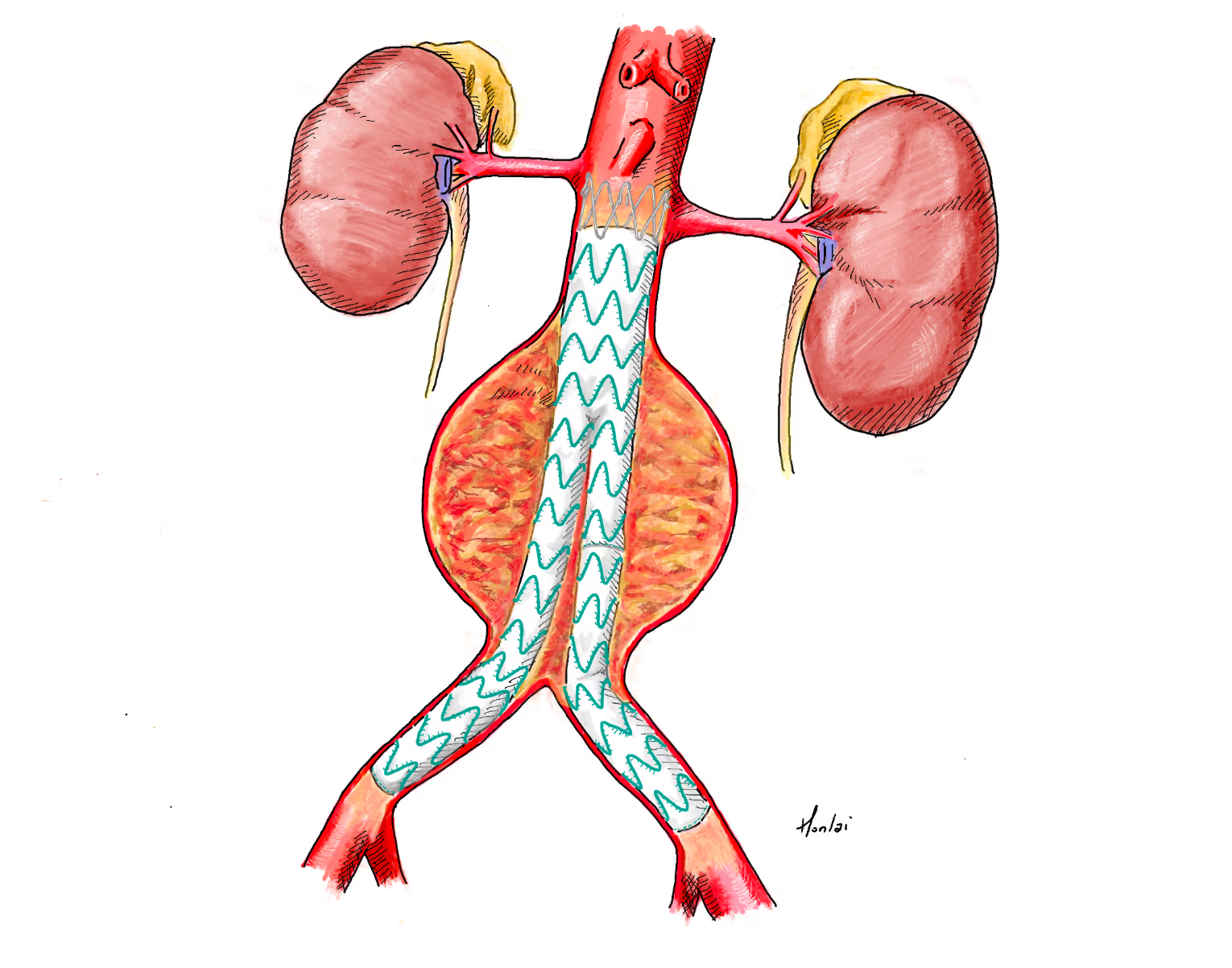
An infrarenal aneurysm,i.e. where there are at least 15mm of non-aneurysmal aorta between the renal arteries and the aneurysm, can usually be treated endovascularly using a standard off-the-shelf stent graft system. However, some additional anatomical conditions must be met for a successful EVAR. These include but are not limited to a cylindrical (as opposed to conical) neck; a neck diameter between 16 and32 (better 28) mm; limited amount of thrombus and calcification in the neck; angulations of the peri- and infrarenal segment within specific limits; a diameter of the aortic bifurcation of at least 16-18mm; iliac arteries that allow the introduction of the delivery systems, are not too kinked and provide adequate sealing zones for the stent grafts.
Educational objectives
.avif)
The Vascular International (VI) School for Vascular Surgery is dedicated to advancing the training and education of vascular surgical techniques through the use of lifelike models. With patient safety as the top priority, VI continuously strives to enhance vascular surgery training, ensuring the highest standards of safe and effective open and endovascular patient care.
About Us